What is a femoral shaft fracture?
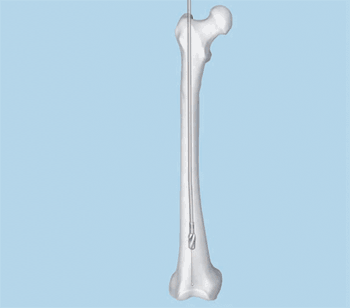
A femoral shaft fracture is a break of the femur (thighbone). Femoral nailing is an operation to fix a broken femur using a metal rod. The metal rod is called a femoral nail (also called an intramedullary or interlocking nail)
Your surgeon has recommended femoral nailing to treat your broken femur. However, it is your decision to go ahead with the operation or not. This document will give you information about the benefits and risks to help you make an informed decision. If you have any questions that this
document does not answer, you should ask your surgeon or any member of the healthcare team.
How does a femoral shaft fracture happen?
Road accidents and sport are the cause of most femoral shaft fractures. You can lose up to a litre (about two pints) of blood into the thigh muscle at the time of the injury. Sometimes the injury causes the bone to break through the skin. This is known as an open or compound fracture.
What are the benefits of surgery?
The main benefits of surgery are that you will only need a short stay in hospital and you will be able to use your leg sooner. Surgery will also make sure your bone heals in a good position.
Are there any alternatives to femoral nailing?
A femoral shaft fracture can be treated in traction (using a heavy weight fixed to the leg to pull the bones into position until they heal). However, some fractures are difficult to hold in a good position without surgery. If you have an open fracture, you will almost certainly need an operation. Your surgeon can sometimes fix your femoral shaft fracture with an external fixator or a plate and screws instead of a femoral nail. They will explain why they recommend femoral nailing for your fracture.
What will happen if I decide not to have the operation?
You will have your leg in traction. You may need to stay in hospital for a long time. This can lead to complications such as blood clots, chest infection and pressure sores. After a number of weeks, your leg may be put into a large plaster cast (called a hip spica) or a brace. The fracture will take about three to six months to heal. You will need physiotherapy to learn to walk again because your muscles will have become weak after spending such a long time in bed.
What does the operation involve?
The healthcare team will carry out a number of checks to make sure you have the operation you came in for and on the correct side. You can help by confirming to your surgeon and the healthcare team your name and the operation you are having.
A variety of anaesthetic techniques is possible. Your anaesthetist will discuss the options with you and recommend the best form of anaesthesia for you. You may also have injections of local anaesthetic to help with the pain after surgery. You may be given antibiotics during the operation to reduce the risk of infection. The operation usually takes between an hour and an hour and a half.
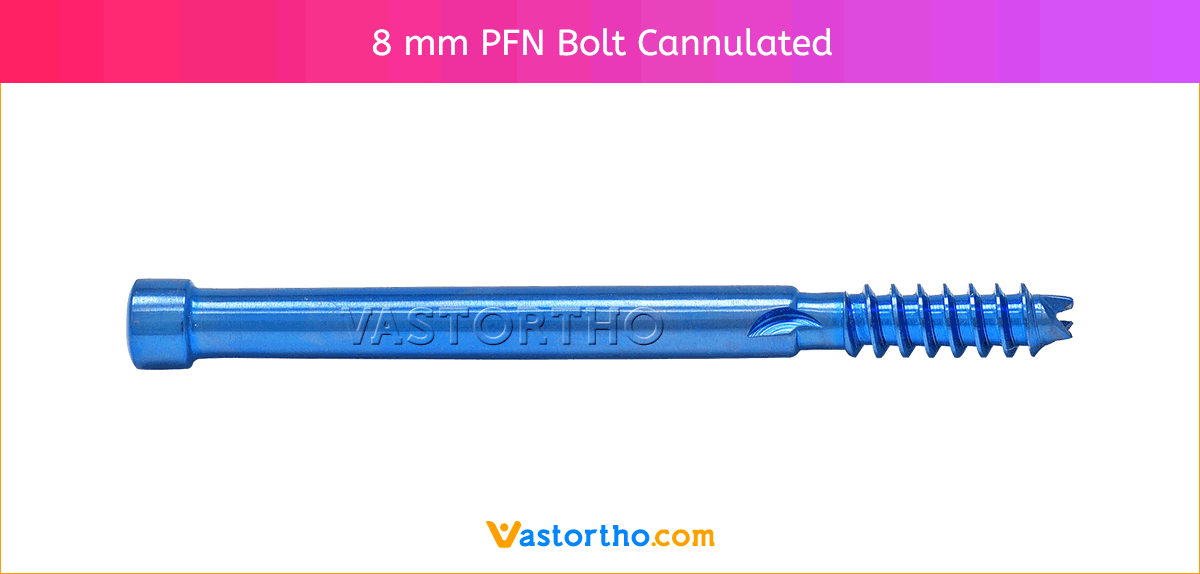
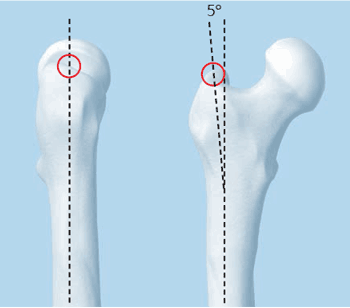
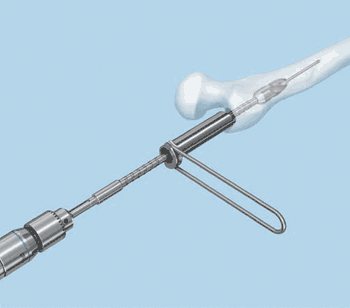
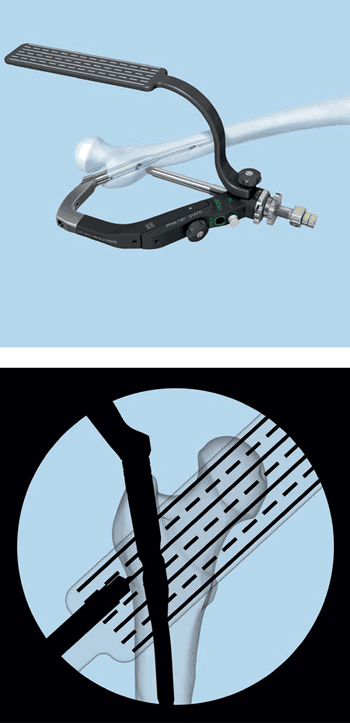
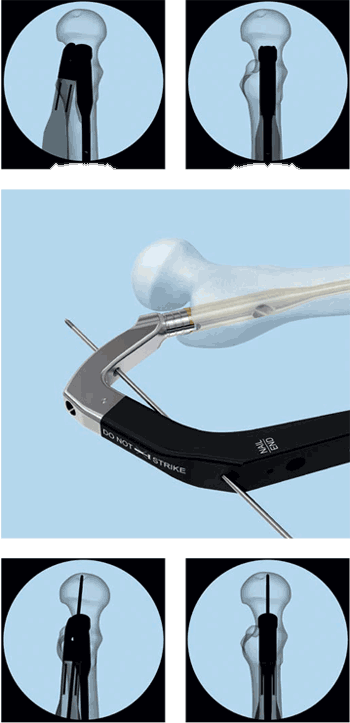
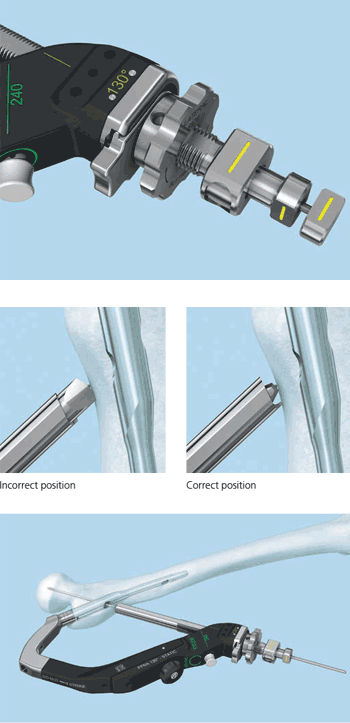
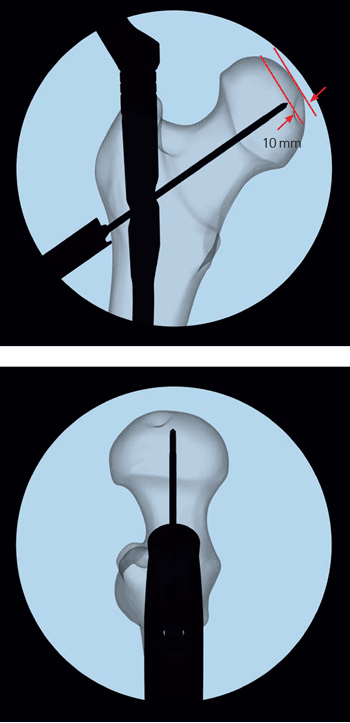
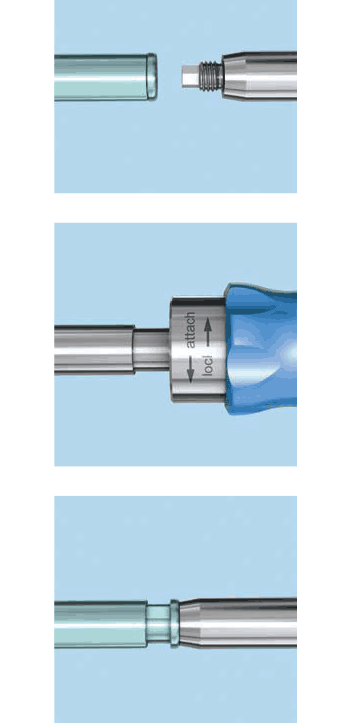
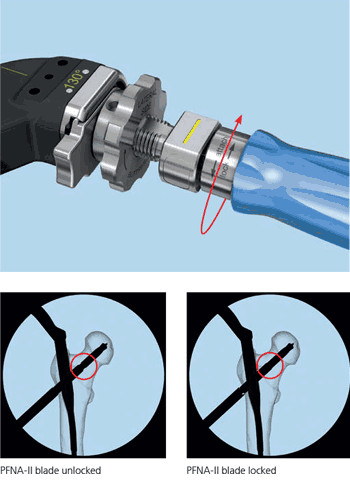
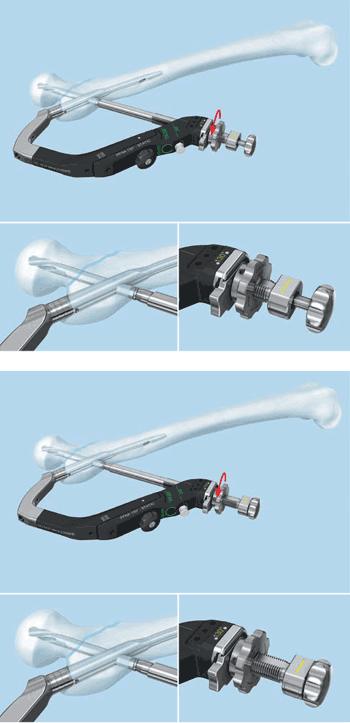
Your surgeon will push the femoral nail down the inside of the bone, either through a cut on the side of the hip or on the front of the knee. The nail goes across the break and holds it in position. The nail is held in the bone by locking screws that pass through holes in the nail. If you have an open fracture, your surgeon will clean the skin wound thoroughly during the operation to reduce the risk of infection. If the skin is badly damaged, you may also need one or more plastic surgery operations. At the end of the operation, your surgeon will close the skin with stitches or clips.
What should I do about my medication?
You should let your doctor know about all the medication you are on and follow their advice. This includes herbal remedies and medication to control diabetes and blood pressure. If you are on beta-blockers, you should continue to take them as normal. You may need to stop taking warfarin or clopidogrel before your operation. Anti-inflammatory painkillers may stop the fracture healing properly, so it is better not to
take these if possible.
What can I do to help make the operation a success?
If you smoke, stopping smoking may reduce your chances of getting complications and will improve your long-term health. Nicotine is known to stop fractures from healing. Regular exercise should help you recover and improve your long-term health. Before you start exercising, ask a member of the healthcare team or your GP for advice. You can reduce your risk of infection in a surgical wound by keeping warm around the time of your operation. Let a member of the healthcare team know if you are cold.