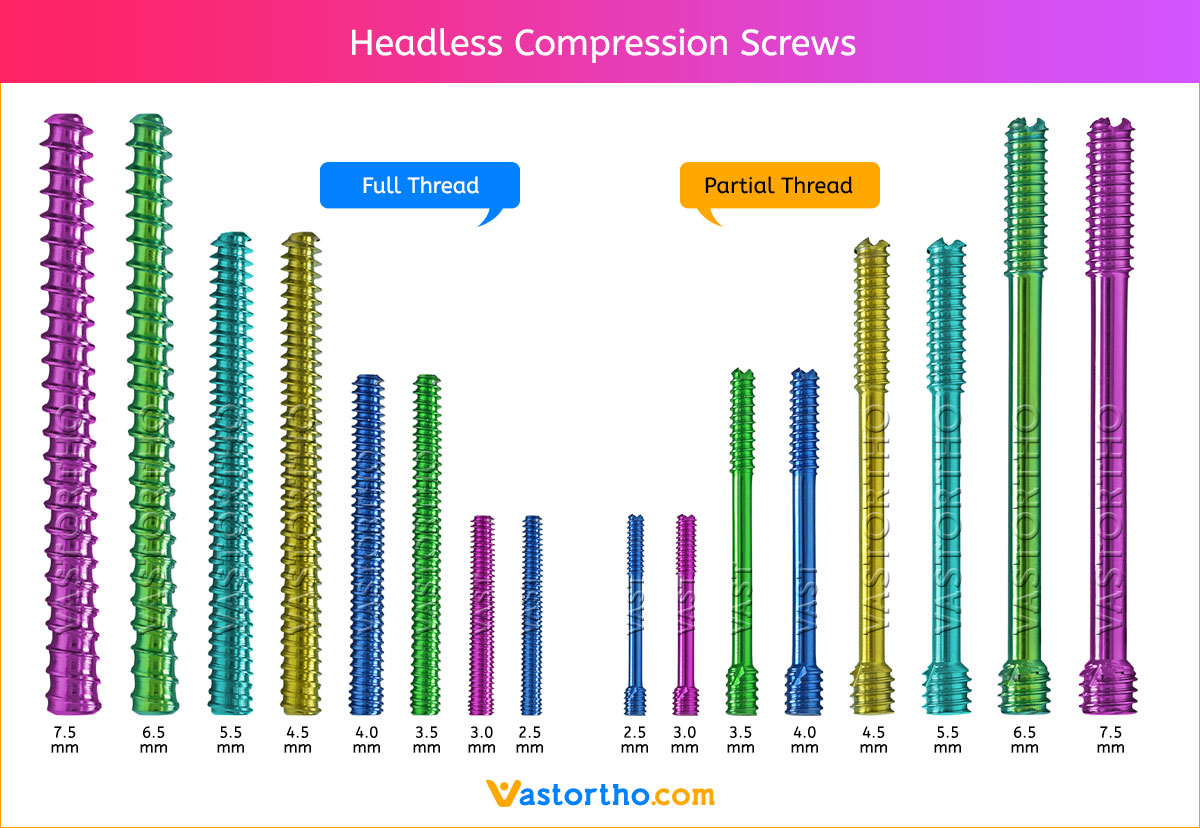
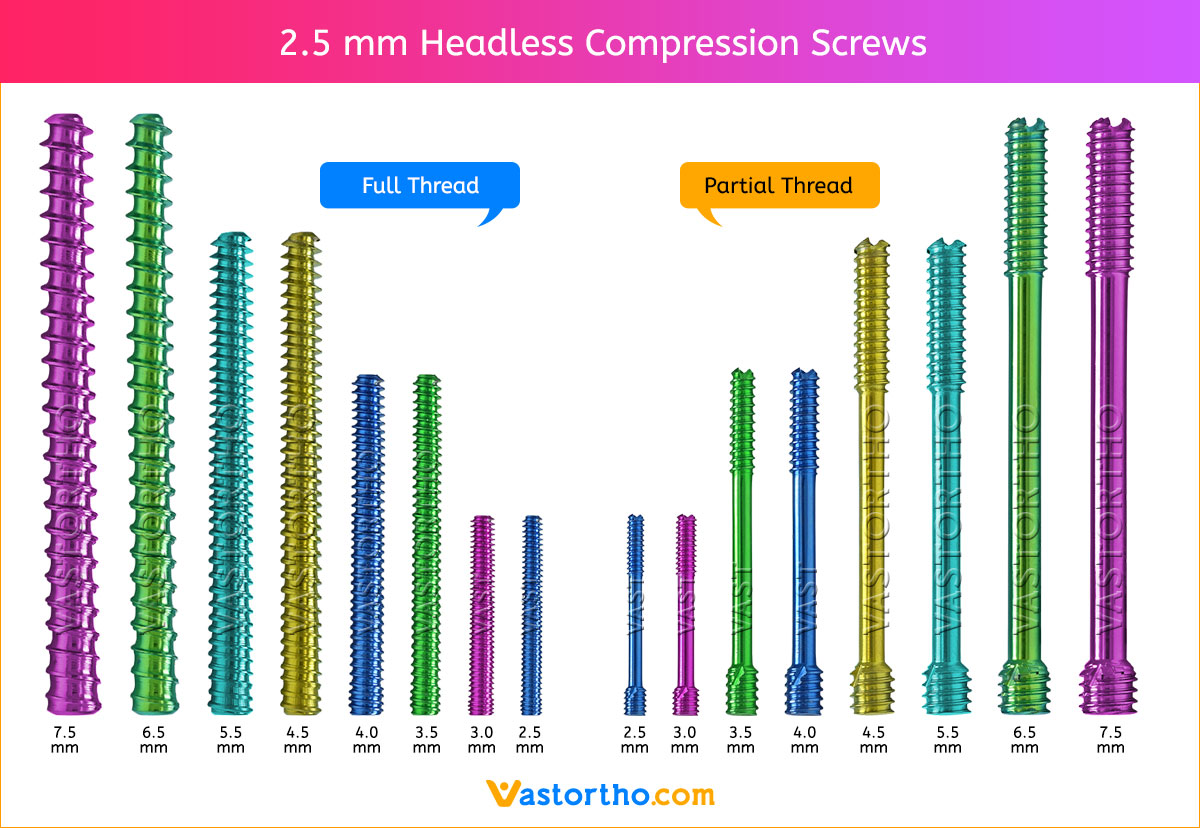
2.5 mm Screws Length
8mm, 10mm, 12mm, 14mm, 16mm, 18mm, 20mm, 22mm, 24mm, 26mm, 28mm and 30mm.
3 mm Screws Length
8mm, 10mm, 12mm, 14mm, 16mm, 18mm, 20mm, 22mm, 24mm, 26mm, 28mm and 30mm.
3.5 mm Screws Length
8mm, 10mm, 12mm, 14mm, 16mm, 18mm, 20mm, 22mm, 24mm, 26mm, 28mm, 30mm, 32mm, 34mm, 36mm, 38mm, 40mm, 42mm, 44mm, 46mm, 48mm, 50mm, 55mm, 60mm, 65mm, 70mm, 75mm and 80mm.
4 mm Screws Length
8mm, 10mm, 12mm, 14mm, 16mm, 18mm, 20mm, 22mm, 24mm, 26mm, 28mm, 30mm, 32mm, 34mm, 36mm, 38mm, 40mm, 42mm, 44mm, 46mm, 48mm, 50mm, 55mm, 60mm, 65mm, 70mm, 75mm and 80mm.
4.5 mm Screws Length
8mm, 10mm, 12mm, 14mm, 16mm, 18mm, 20mm, 22mm, 24mm, 26mm, 28mm, 30mm, 32mm, 34mm, 36mm, 38mm, 40mm, 42mm, 44mm, 46mm, 48mm, 50mm, 55mm, 60mm, 65mm, 70mm, 75mm and 80mm.
5.5 mm Screws Length
12mm, 14mm, 16mm, 18mm, 20mm, 22mm, 24mm, 26mm, 28mm, 30mm, 32mm, 34mm, 36mm, 38mm, 40mm, 42mm, 44mm, 46mm, 48mm, 50mm, 55mm, 60mm, 65mm, 70mm, 75mm, 80mm, 85mm, 90mm, 95mm, 100mm, 105mm, 110mm, 115mm and 120mm.
6.5 mm Screws Length
12mm, 14mm, 16mm, 18mm, 20mm, 22mm, 24mm, 26mm, 28mm, 30mm, 32mm, 34mm, 36mm, 38mm, 40mm, 42mm, 44mm, 46mm, 48mm, 50mm, 55mm, 60mm, 65mm, 70mm, 75mm, 80mm, 85mm, 90mm, 95mm, 100mm, 105mm, 110mm, 115mm and 120mm.
7.5 mm Screws Length
12mm, 14mm, 16mm, 18mm, 20mm, 22mm, 24mm, 26mm, 28mm, 30mm, 32mm, 34mm, 36mm, 38mm, 40mm, 42mm, 44mm, 46mm, 48mm, 50mm, 55mm, 60mm, 65mm, 70mm, 75mm, 80mm, 85mm, 90mm, 95mm, 100mm, 105mm, 110mm, 115mm and 120mm.
 https://www.vastortho.com/wp-content/uploads/2.5-mm-Headless-Compression-Screws.jpg
828
1200
VastOrtho
https://www.vastortho.com/wp-content/uploads/Vast-Ortho-Logo-for-website.png
VastOrtho2018-08-27 13:09:322023-07-22 12:57:592.5 mm Headless Compression Screw
https://www.vastortho.com/wp-content/uploads/2.5-mm-Headless-Compression-Screws.jpg
828
1200
VastOrtho
https://www.vastortho.com/wp-content/uploads/Vast-Ortho-Logo-for-website.png
VastOrtho2018-08-27 13:09:322023-07-22 12:57:592.5 mm Headless Compression Screw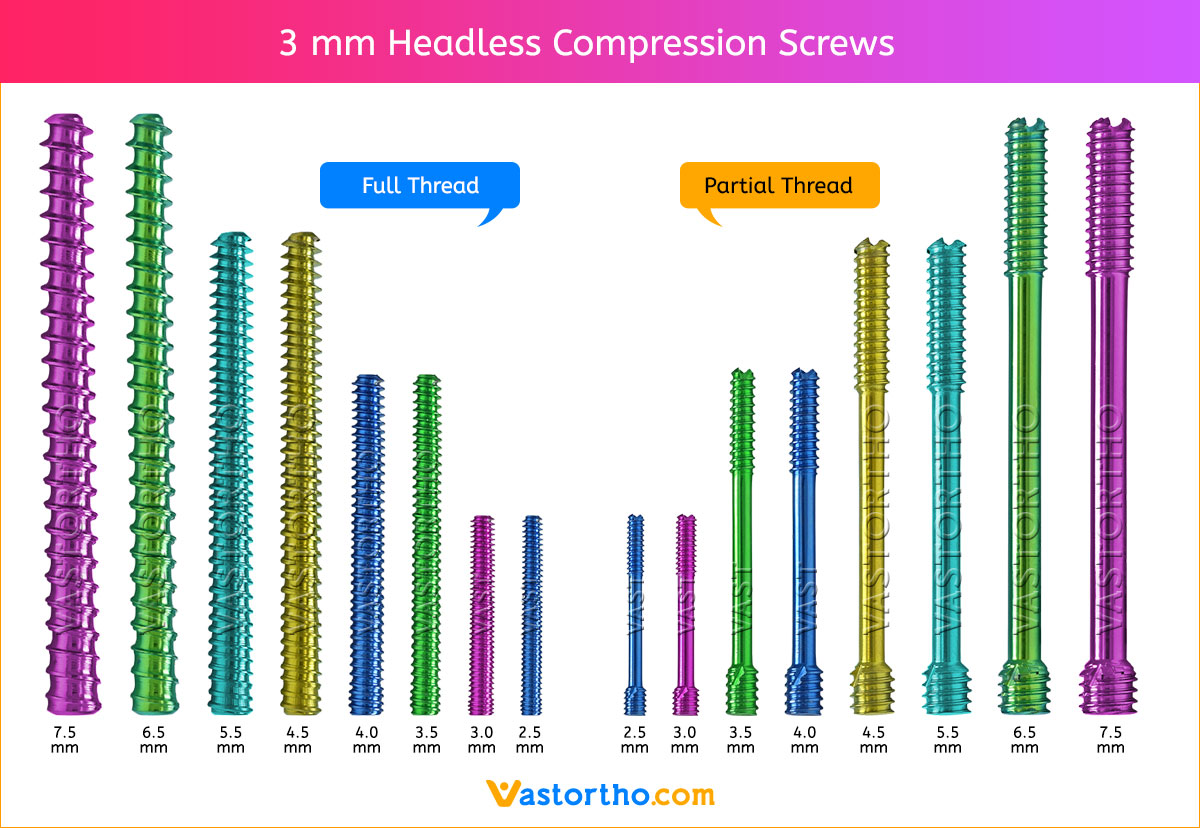 https://www.vastortho.com/wp-content/uploads/3-mm-Headless-Compression-Screws.jpg
828
1200
VastOrtho
https://www.vastortho.com/wp-content/uploads/Vast-Ortho-Logo-for-website.png
VastOrtho2018-08-27 13:07:552023-07-22 13:00:153 mm Headless Compression Screw
https://www.vastortho.com/wp-content/uploads/3-mm-Headless-Compression-Screws.jpg
828
1200
VastOrtho
https://www.vastortho.com/wp-content/uploads/Vast-Ortho-Logo-for-website.png
VastOrtho2018-08-27 13:07:552023-07-22 13:00:153 mm Headless Compression Screw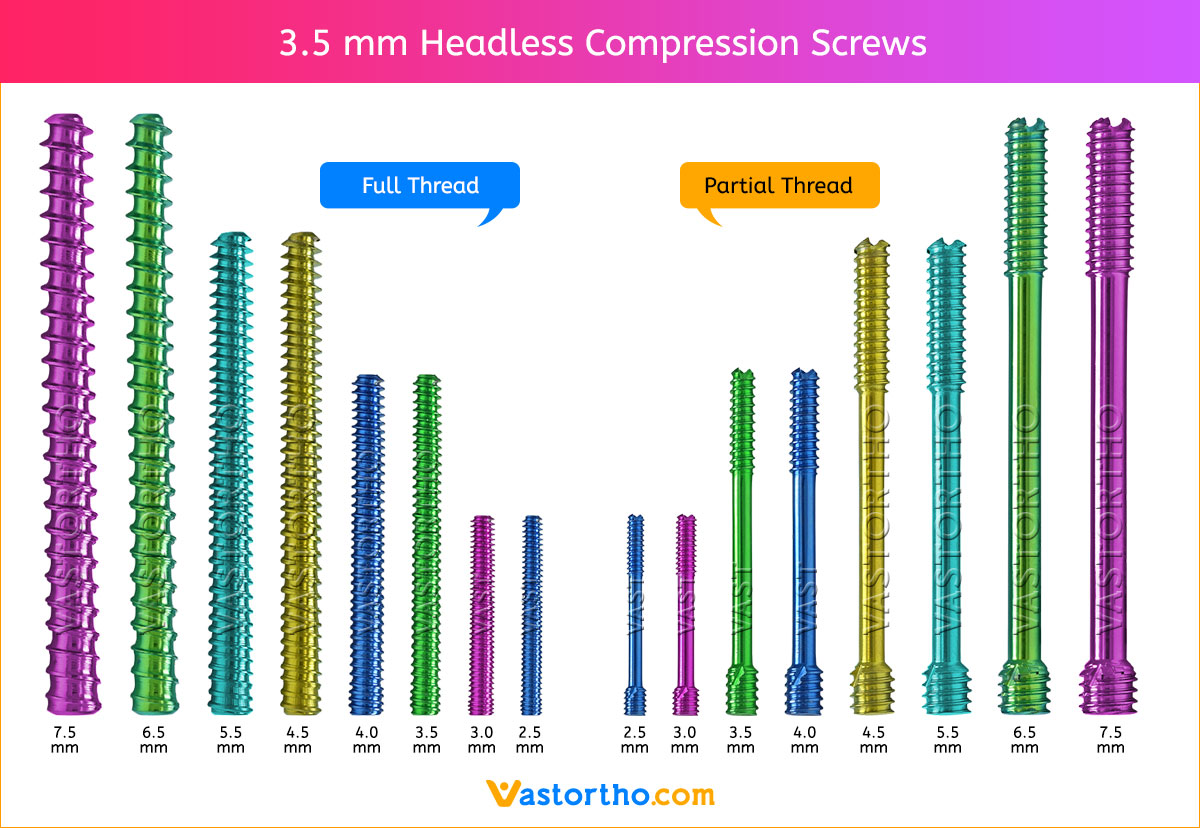 https://www.vastortho.com/wp-content/uploads/3.5-mm-Headless-Compression-Screws.jpg
828
1200
VastOrtho
https://www.vastortho.com/wp-content/uploads/Vast-Ortho-Logo-for-website.png
VastOrtho2018-08-26 17:44:092023-07-22 13:01:483.5 mm Headless Compression Screw
https://www.vastortho.com/wp-content/uploads/3.5-mm-Headless-Compression-Screws.jpg
828
1200
VastOrtho
https://www.vastortho.com/wp-content/uploads/Vast-Ortho-Logo-for-website.png
VastOrtho2018-08-26 17:44:092023-07-22 13:01:483.5 mm Headless Compression Screw https://www.vastortho.com/wp-content/uploads/4-mm-Headless-Compression-Screws.jpg
828
1200
VastOrtho
https://www.vastortho.com/wp-content/uploads/Vast-Ortho-Logo-for-website.png
VastOrtho2018-08-25 17:54:302023-07-22 17:10:034 mm Headless Compression Screw
https://www.vastortho.com/wp-content/uploads/4-mm-Headless-Compression-Screws.jpg
828
1200
VastOrtho
https://www.vastortho.com/wp-content/uploads/Vast-Ortho-Logo-for-website.png
VastOrtho2018-08-25 17:54:302023-07-22 17:10:034 mm Headless Compression Screw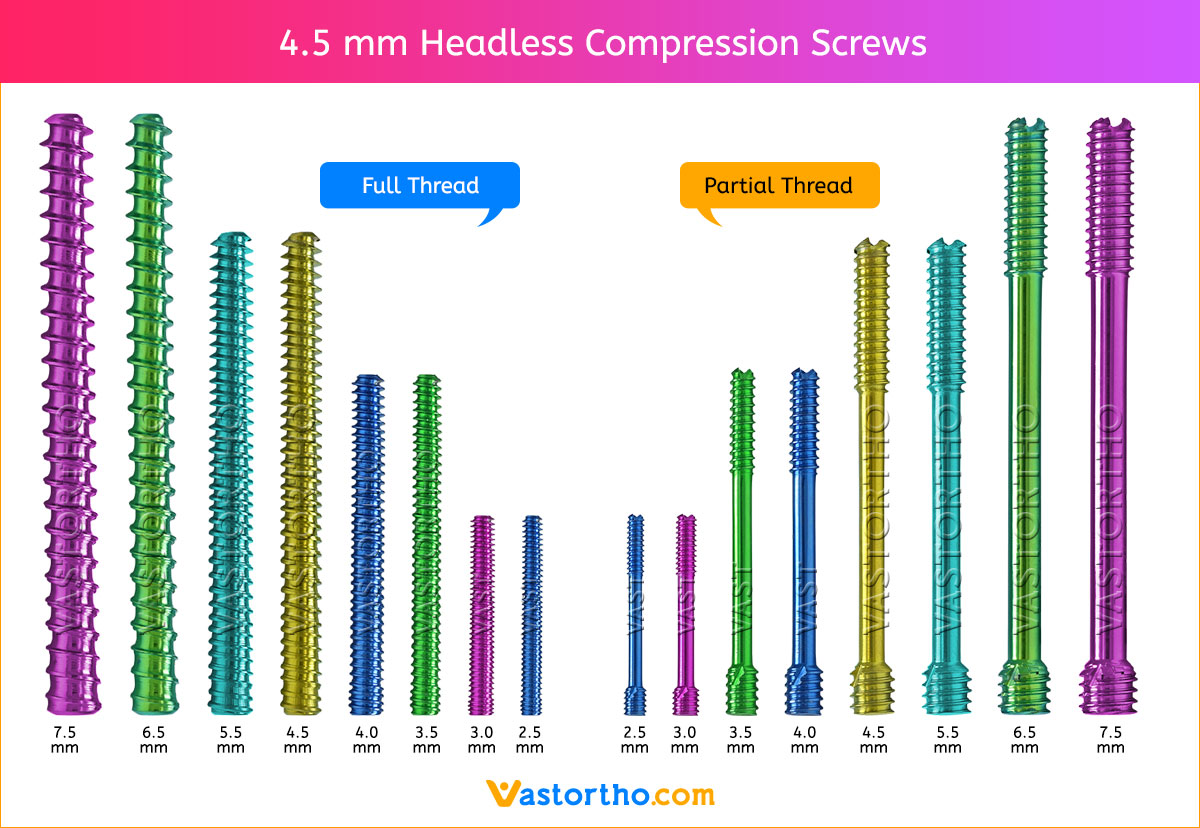 https://www.vastortho.com/wp-content/uploads/4.5-mm-Headless-Compression-Screws.jpg
828
1200
VastOrtho
https://www.vastortho.com/wp-content/uploads/Vast-Ortho-Logo-for-website.png
VastOrtho2018-08-25 17:50:132023-07-22 17:15:494.5 mm Headless Compression Screw
https://www.vastortho.com/wp-content/uploads/4.5-mm-Headless-Compression-Screws.jpg
828
1200
VastOrtho
https://www.vastortho.com/wp-content/uploads/Vast-Ortho-Logo-for-website.png
VastOrtho2018-08-25 17:50:132023-07-22 17:15:494.5 mm Headless Compression Screw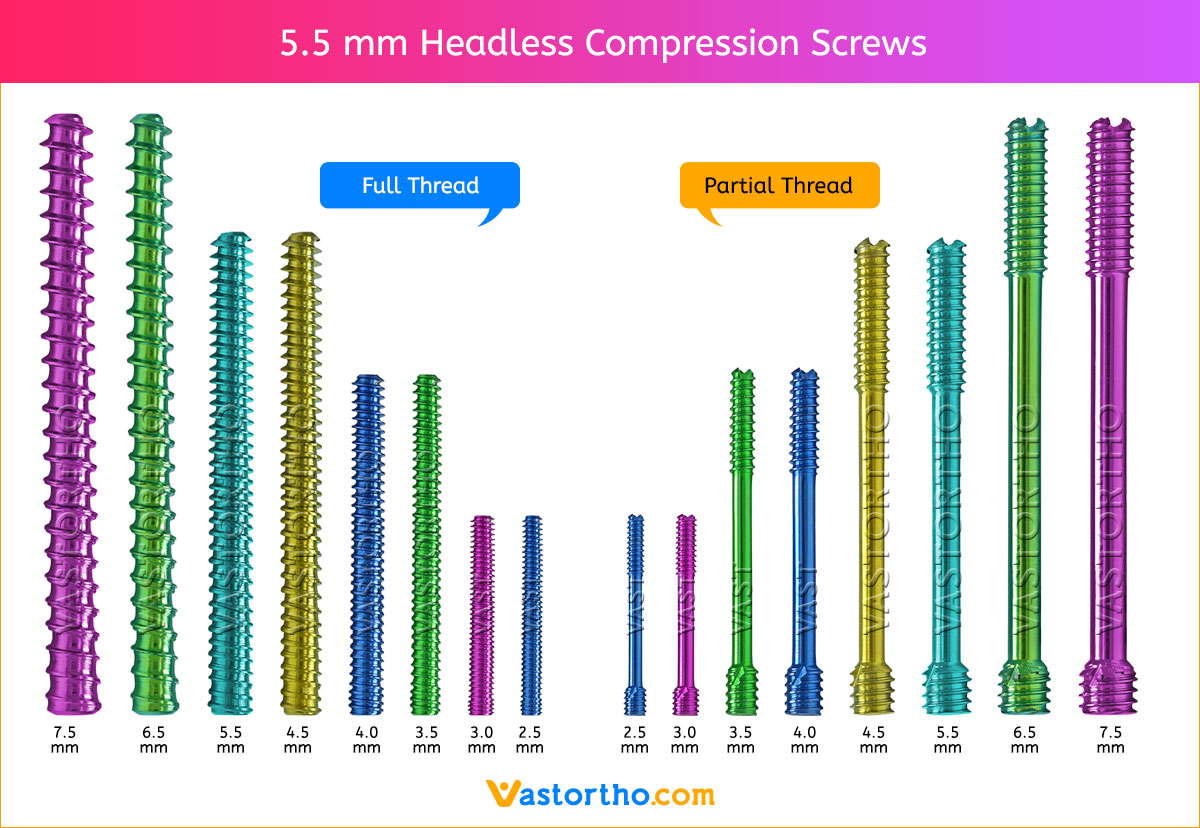 https://www.vastortho.com/wp-content/uploads/5.5-mm-Headless-Compression-Screws.jpg
828
1200
VastOrtho
https://www.vastortho.com/wp-content/uploads/Vast-Ortho-Logo-for-website.png
VastOrtho2018-08-23 23:51:542023-07-22 17:17:575.5 mm Headless Compression Screw
https://www.vastortho.com/wp-content/uploads/5.5-mm-Headless-Compression-Screws.jpg
828
1200
VastOrtho
https://www.vastortho.com/wp-content/uploads/Vast-Ortho-Logo-for-website.png
VastOrtho2018-08-23 23:51:542023-07-22 17:17:575.5 mm Headless Compression Screw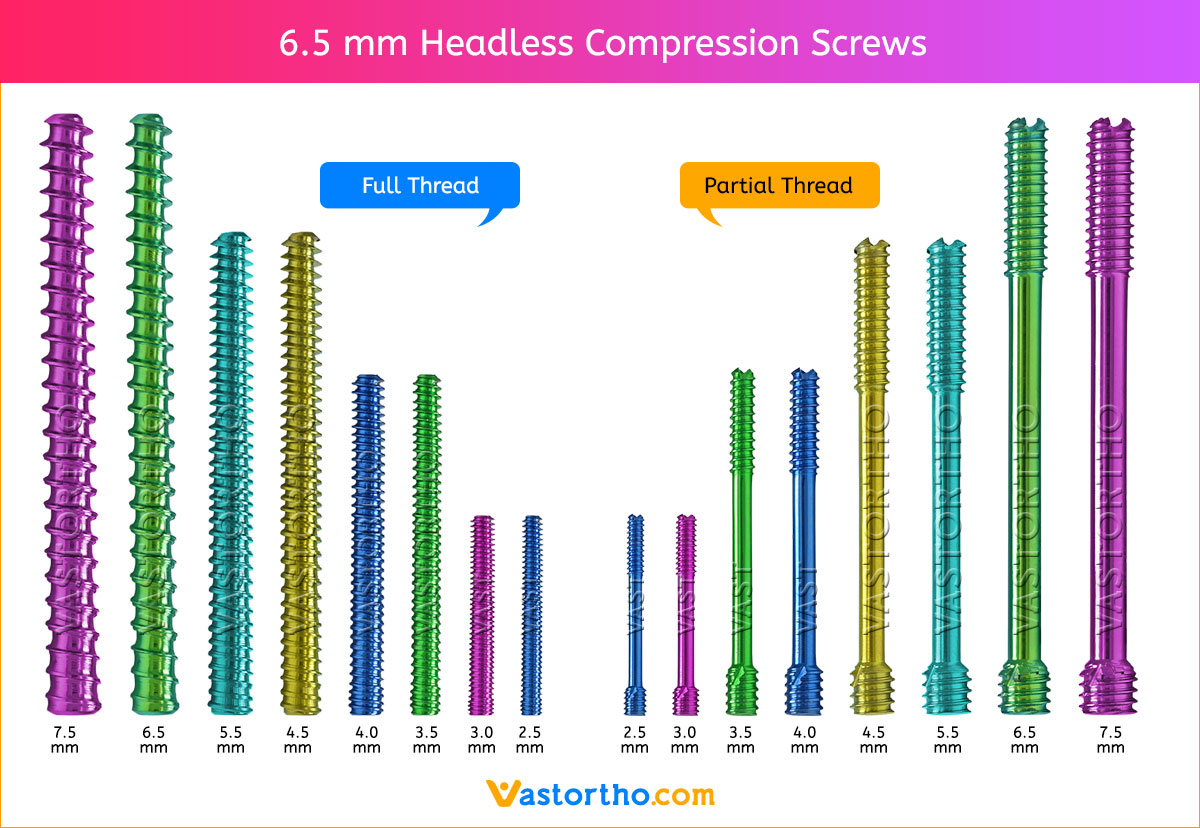 https://www.vastortho.com/wp-content/uploads/6.5-mm-Headless-Compression-Screws.jpg
828
1200
VastOrtho
https://www.vastortho.com/wp-content/uploads/Vast-Ortho-Logo-for-website.png
VastOrtho2018-08-18 17:19:472023-07-22 17:22:526.5 mm Headless Compression Screw
https://www.vastortho.com/wp-content/uploads/6.5-mm-Headless-Compression-Screws.jpg
828
1200
VastOrtho
https://www.vastortho.com/wp-content/uploads/Vast-Ortho-Logo-for-website.png
VastOrtho2018-08-18 17:19:472023-07-22 17:22:526.5 mm Headless Compression Screw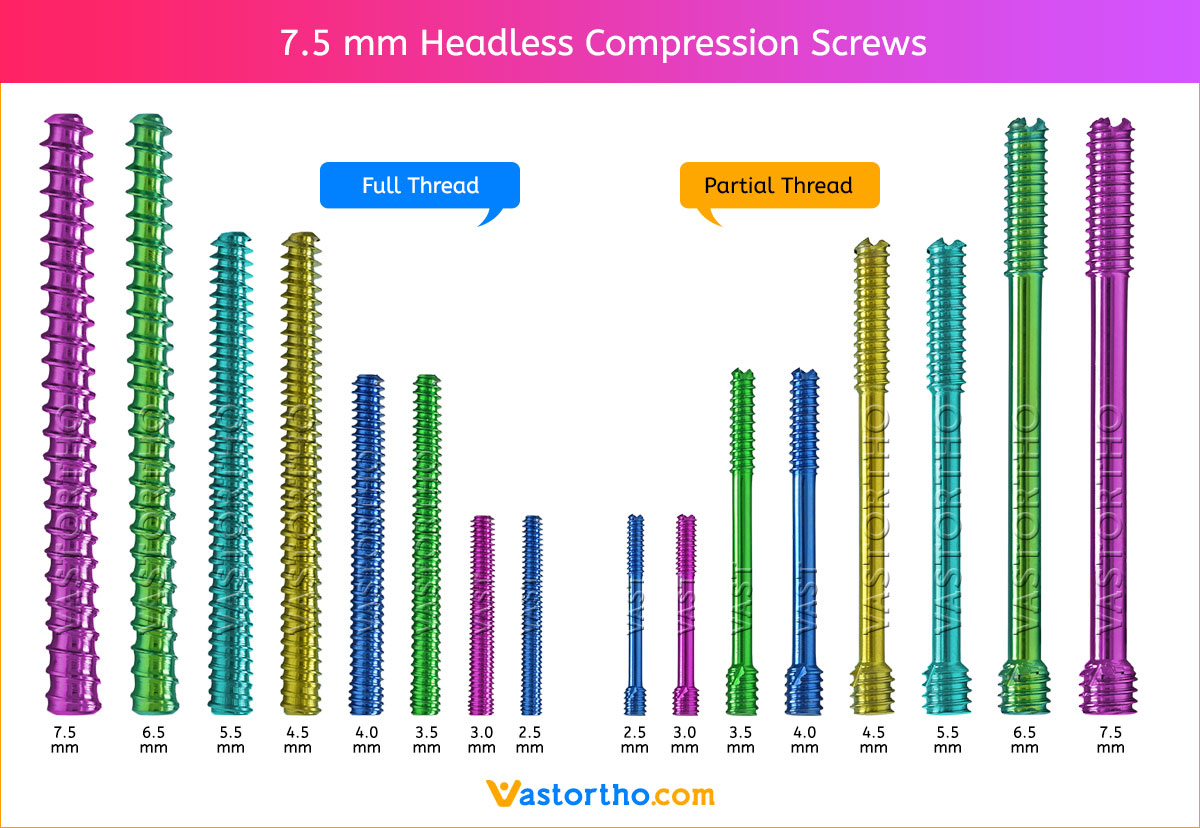 https://www.vastortho.com/wp-content/uploads/7.5-mm-Headless-Compression-Screws.jpg
828
1200
VastOrtho
https://www.vastortho.com/wp-content/uploads/Vast-Ortho-Logo-for-website.png
VastOrtho2018-08-17 12:01:172023-07-22 17:26:357.5 mm Headless Compression Screw
https://www.vastortho.com/wp-content/uploads/7.5-mm-Headless-Compression-Screws.jpg
828
1200
VastOrtho
https://www.vastortho.com/wp-content/uploads/Vast-Ortho-Logo-for-website.png
VastOrtho2018-08-17 12:01:172023-07-22 17:26:357.5 mm Headless Compression Screw